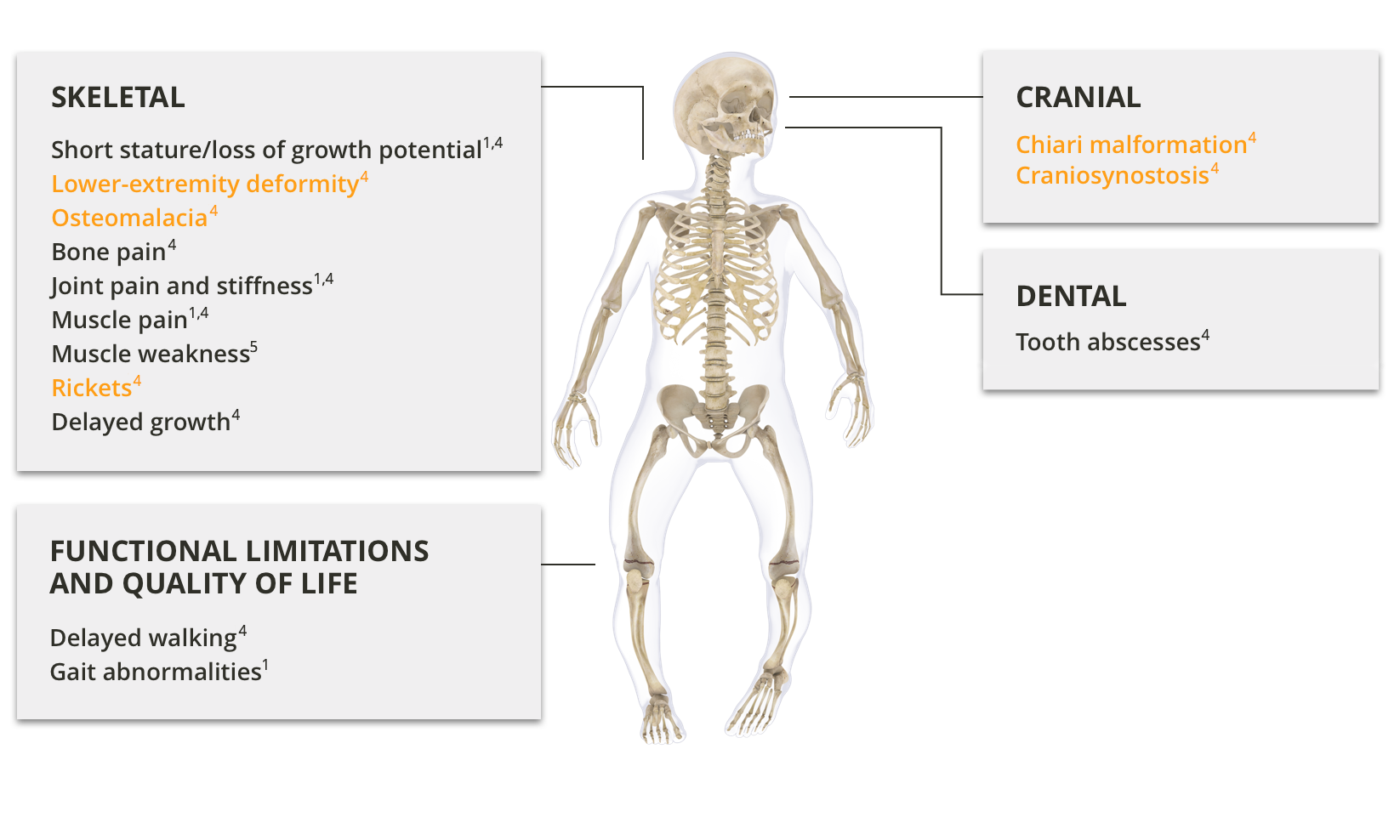
Clinical manifestations in paediatric patients with XLH
XLH causes lifelong skeletal disease and can substantially decrease physical function and quality of life1
XLH typically presents during the first 2 years of life with progressive lower-extremity bowing, impaired growth after the onset of weight bearing, and the characteristic clinical signs of rickets. Pain, gait disturbances, and impaired gross motor function may also be observed.2,3

Children with XLH suffer from poor quality of life, impaired mobility, and bone and joint pain.1
In addition to skeletal disease and impaired growth, children with XLH may also have dental manifestations of the disease.1,4
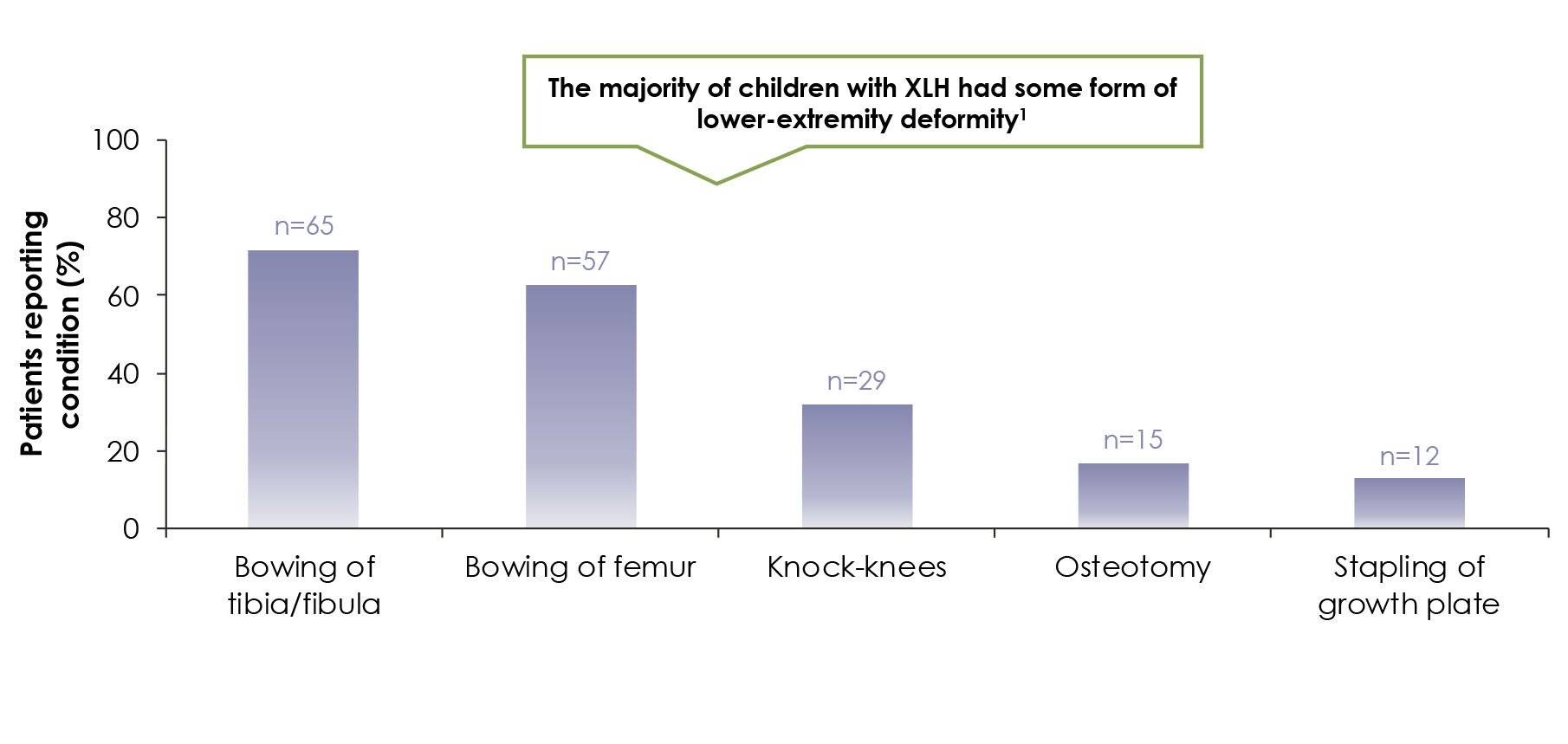
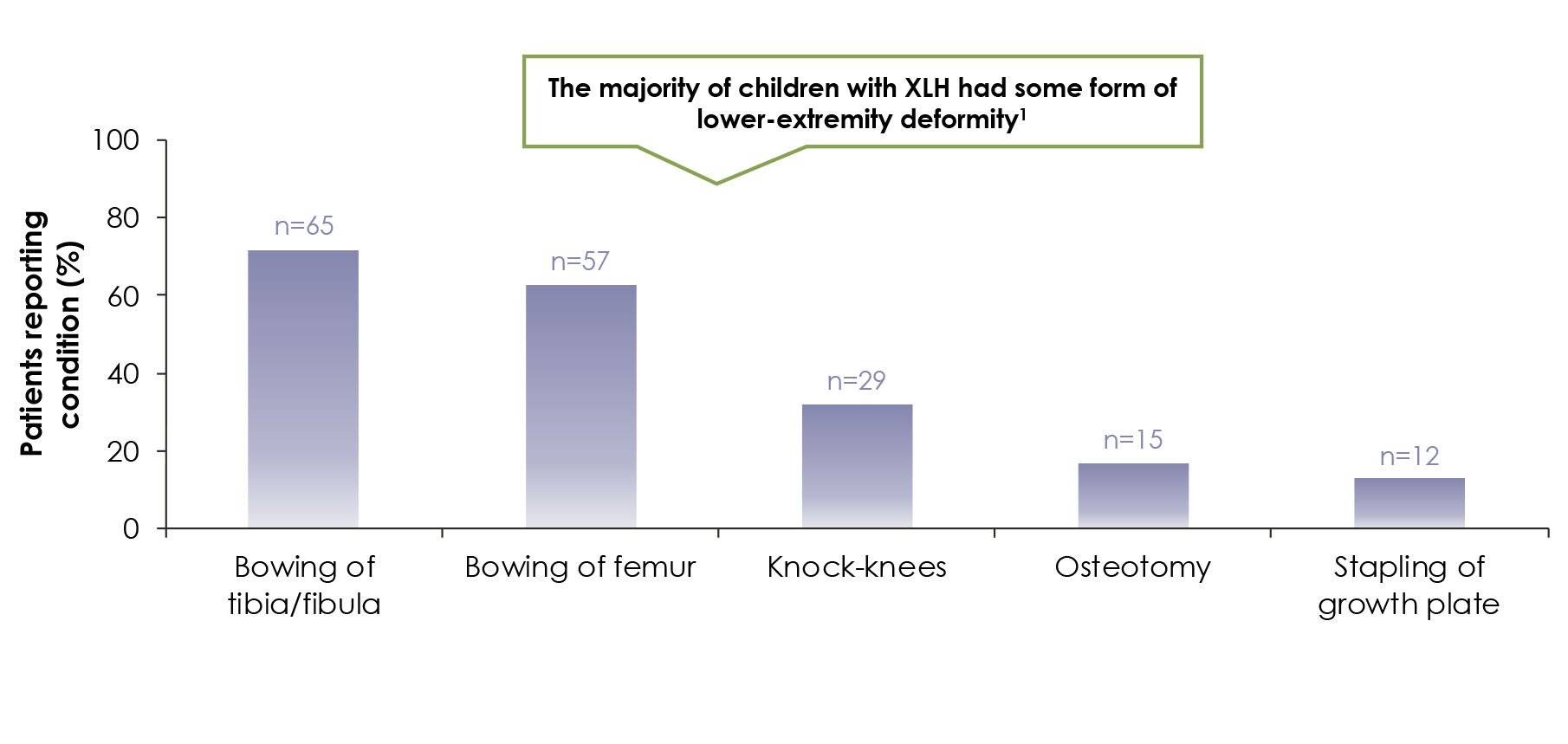
In a survey of 90 children with XLH, lower-extremity deformities were reported in most children , with ~47% receiving corrective surgery1
Growth
Children with XLH are prone to growth impairment, and linear body dimensions are significantly reduced compared to those of healthy children at all ages.10
Paediatric XLH patients show impaired growth compared to non-XLH children1,4
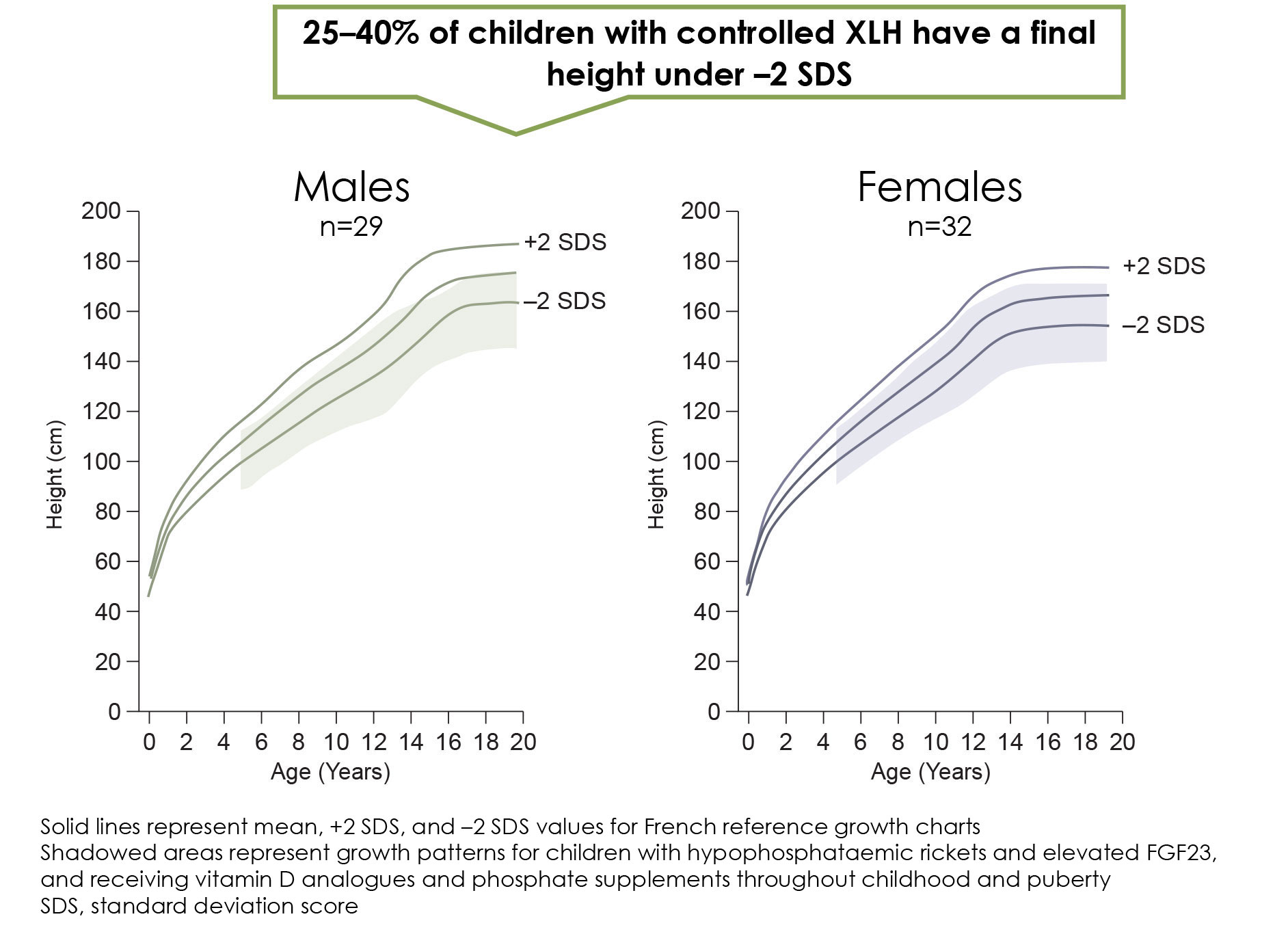
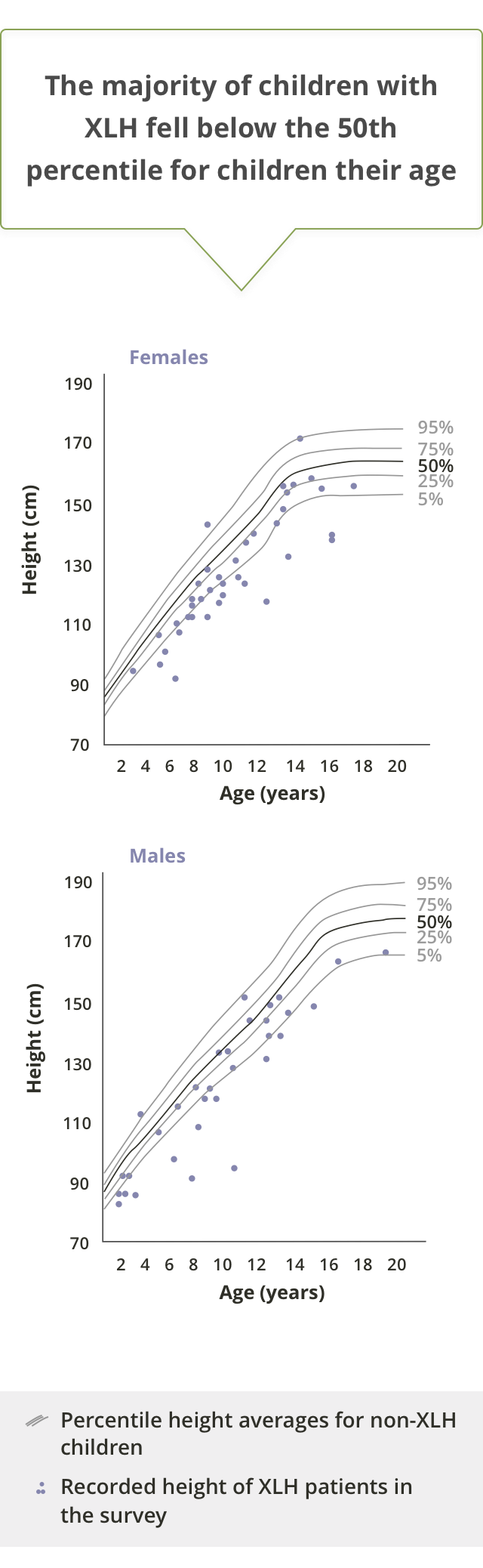
Stature, sitting height, and arm and leg length over time in children with XLH versus normal population10
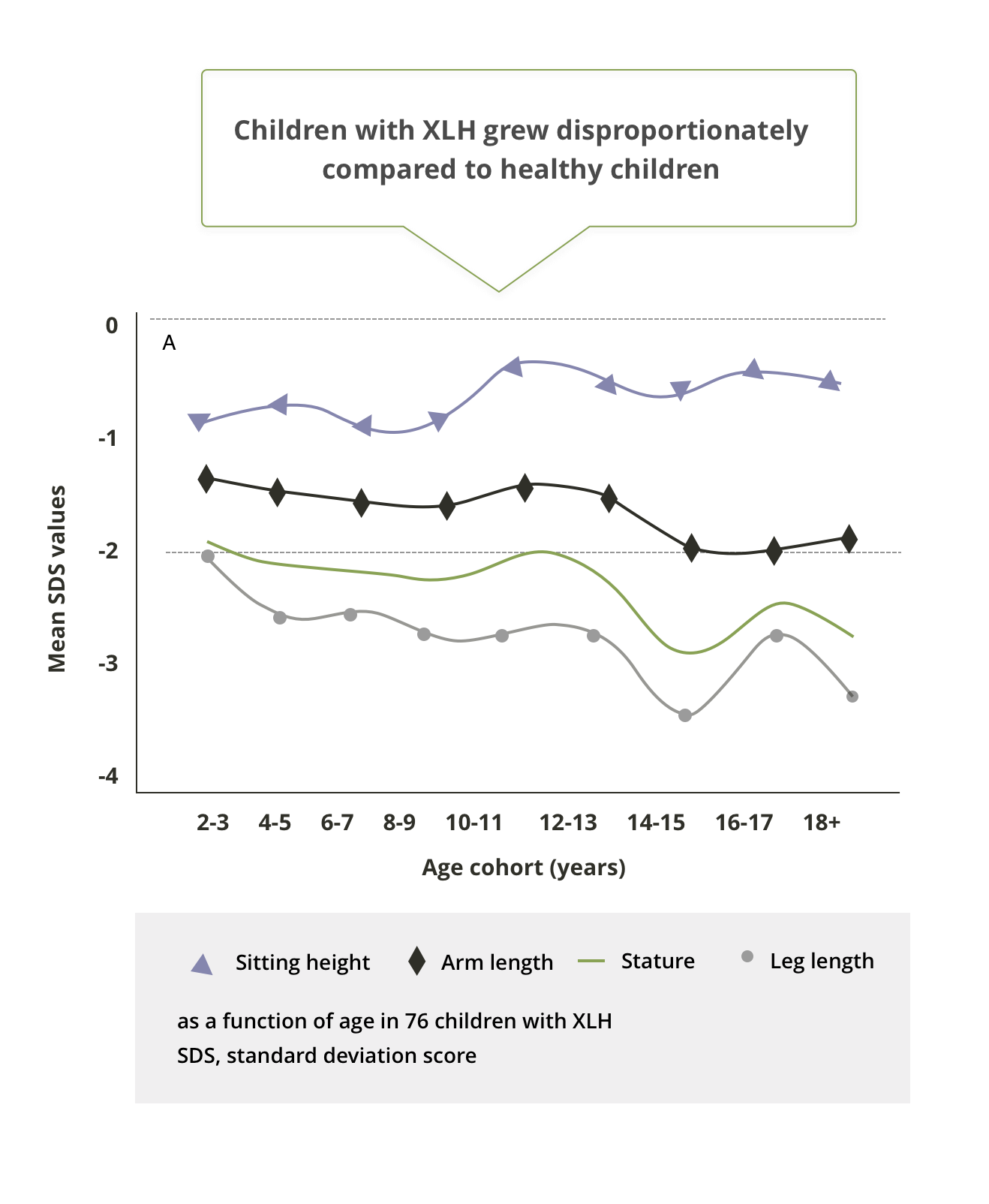
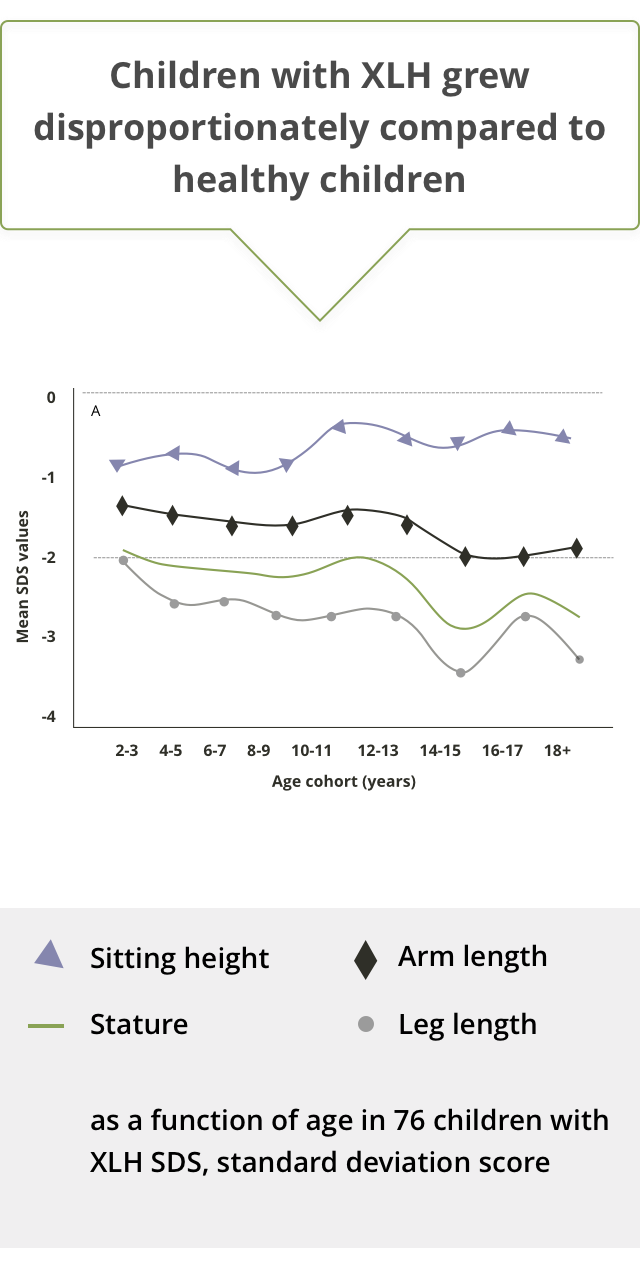
While linear body dimensions are significantly reduced compared to those of normal children at all ages, there is a strong association between stature and leg length in paediatric XLH patients.10
Generally, leg length decreases progressively during childhood and adolescence, while sitting height increases significantly during late childhood.10
Dental Manifestations
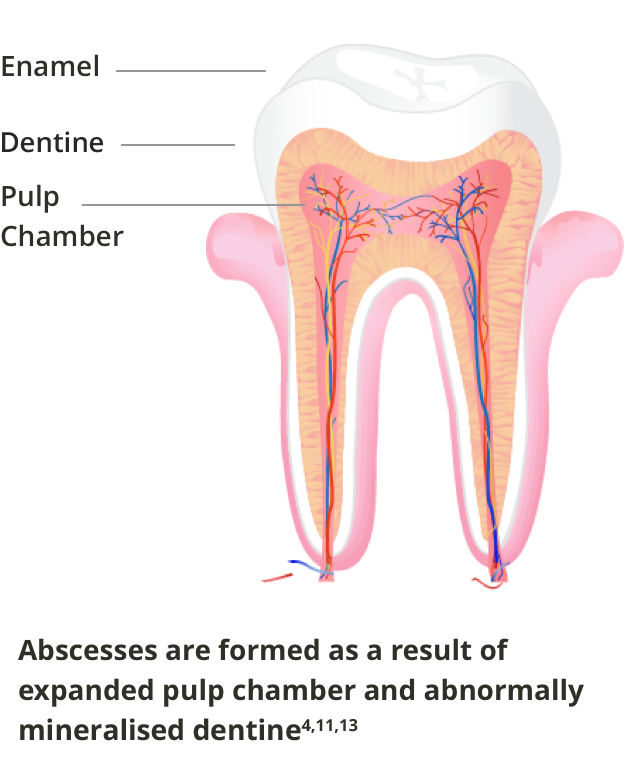
XLH patients can be affected by tooth abscesses in both deciduous and permanent dentition. The disease results in a diminished barrier to the exterior of the tooth, with cracks in the thin enamel, extended pulp horns, and abnormal formation of the dentine, allowing bacteria and infections to enter the tooth pulp chamber without any visible damage to the tooth.4,11
In an international online survey of parents/caregivers of 90 children with XLH aged 0 to 18 years, it was found that 51% of children had dental abscesses.1

Spontaneous abscesses appear as a result of bacterial invasion into the expanded pulp chamber via the thin and fissured enamel and abnormally mineralised and malformed dentine.4,11
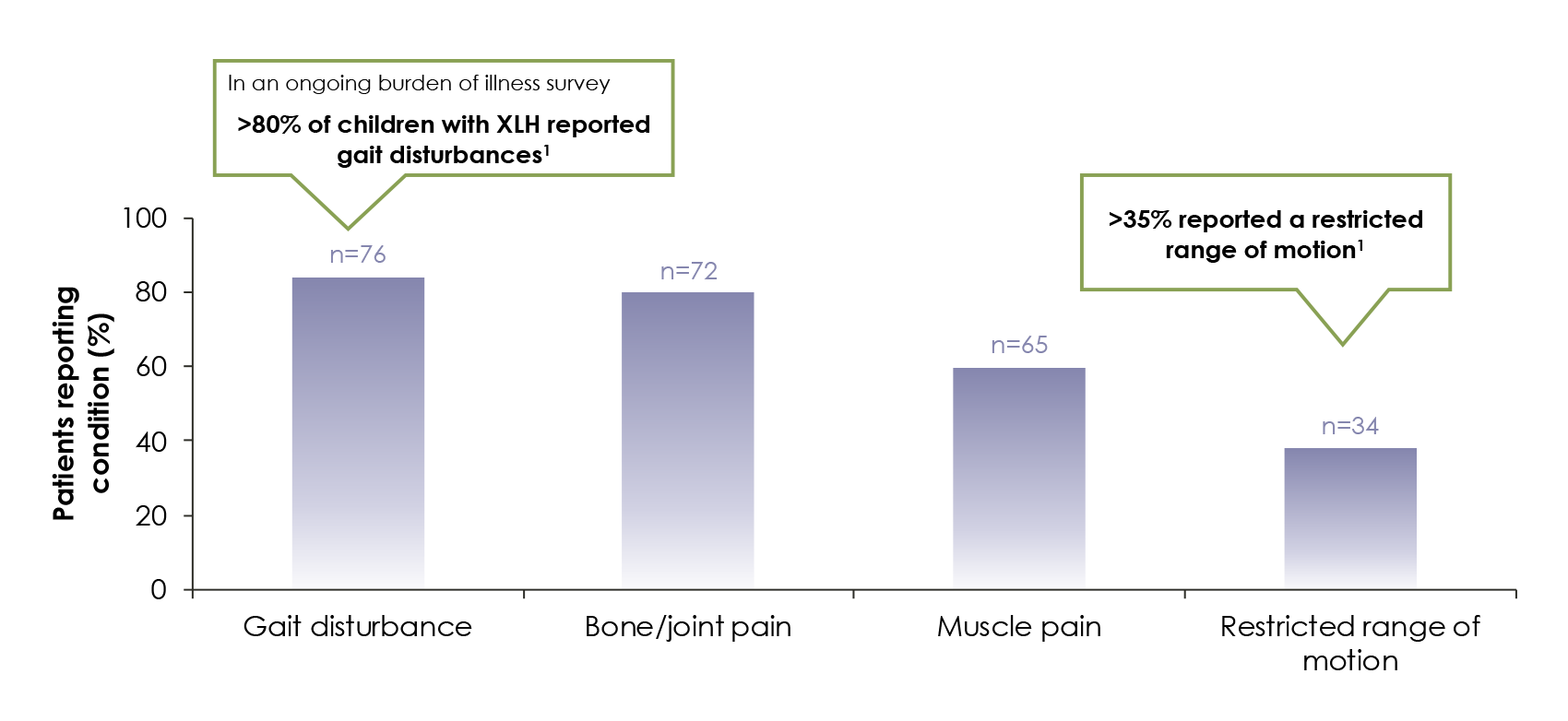
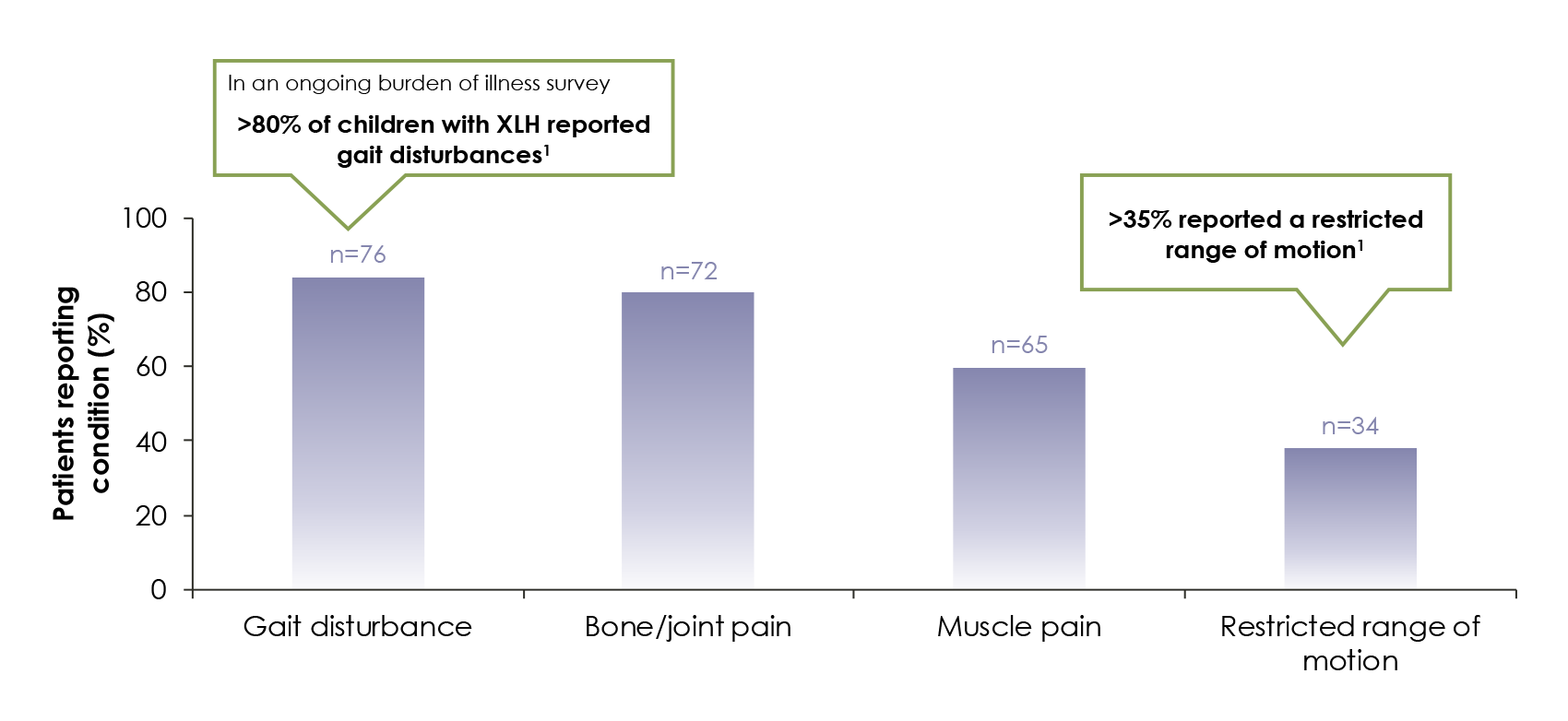
Children with XLH can experience diminished mobility
and functional limitations4
In children with XLH, lower-extremity muscle strength and walking ability are substantially decreased relative to non-XLH children.5
Commonly reported functional limitations and pain in 90 paediatric XLH patients1
Children with XLH can have impaired quality of life (QOL)1
Skeletal manifestations of XLH impact physical and psychosocial quality of life in paediatric patients.1
Added to this, many XLH children experience regular joint pain.1
Over 55% of children with XLH report knee pain. Pain is also commonly experienced in the1
- Feet
- Hips
- Ankles
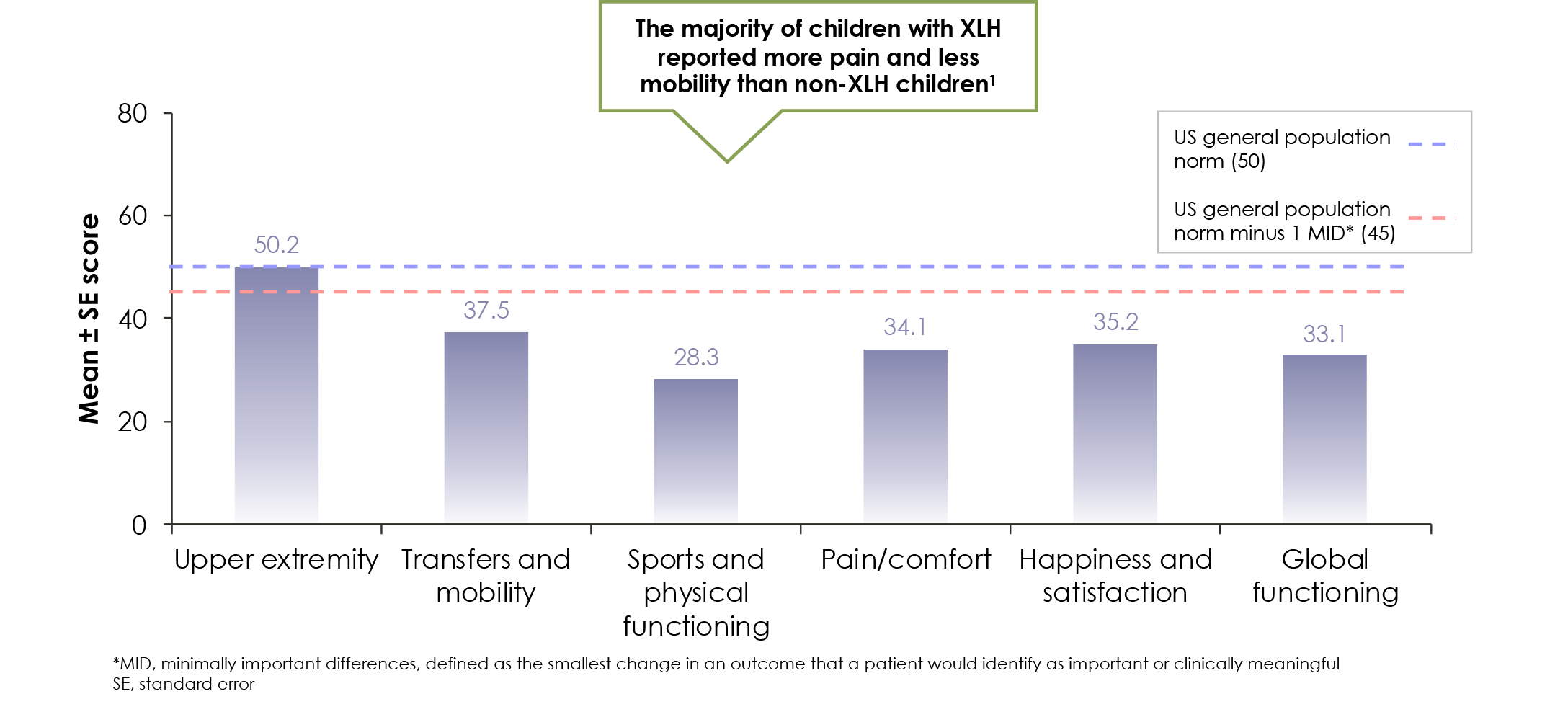
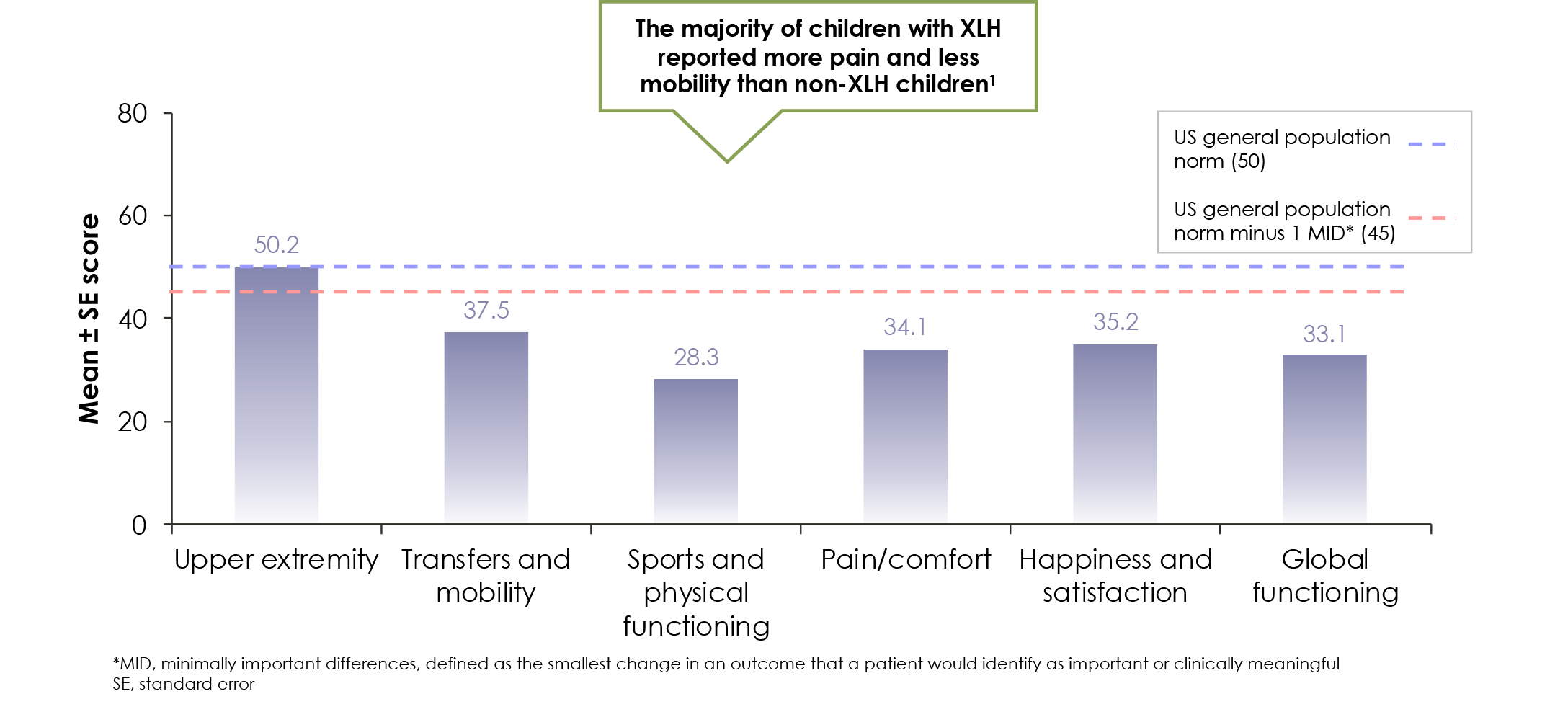
In an international survey, 90 children with XLH had mean health-related quality of life scores below the normal mean for the general US population1
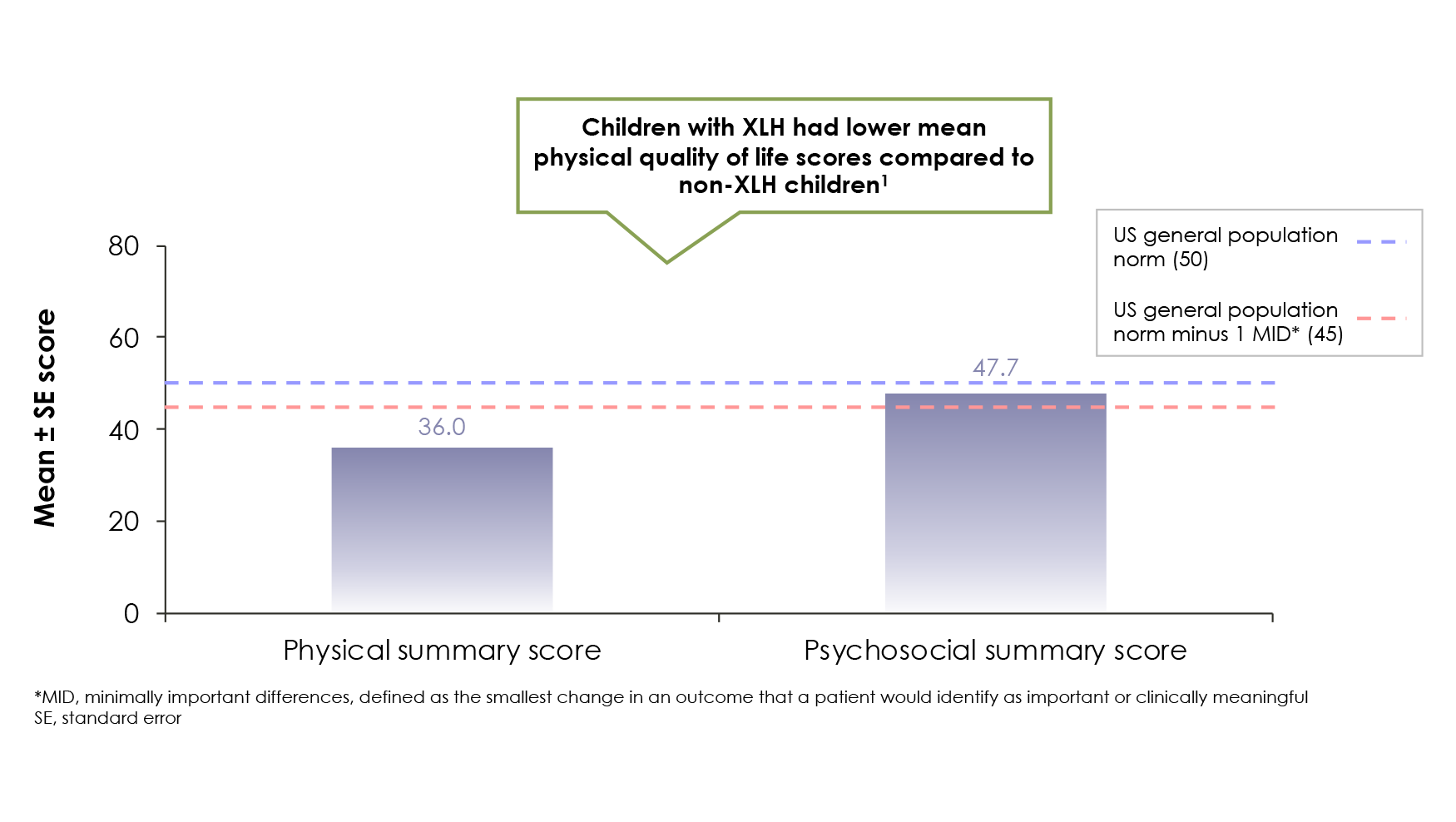
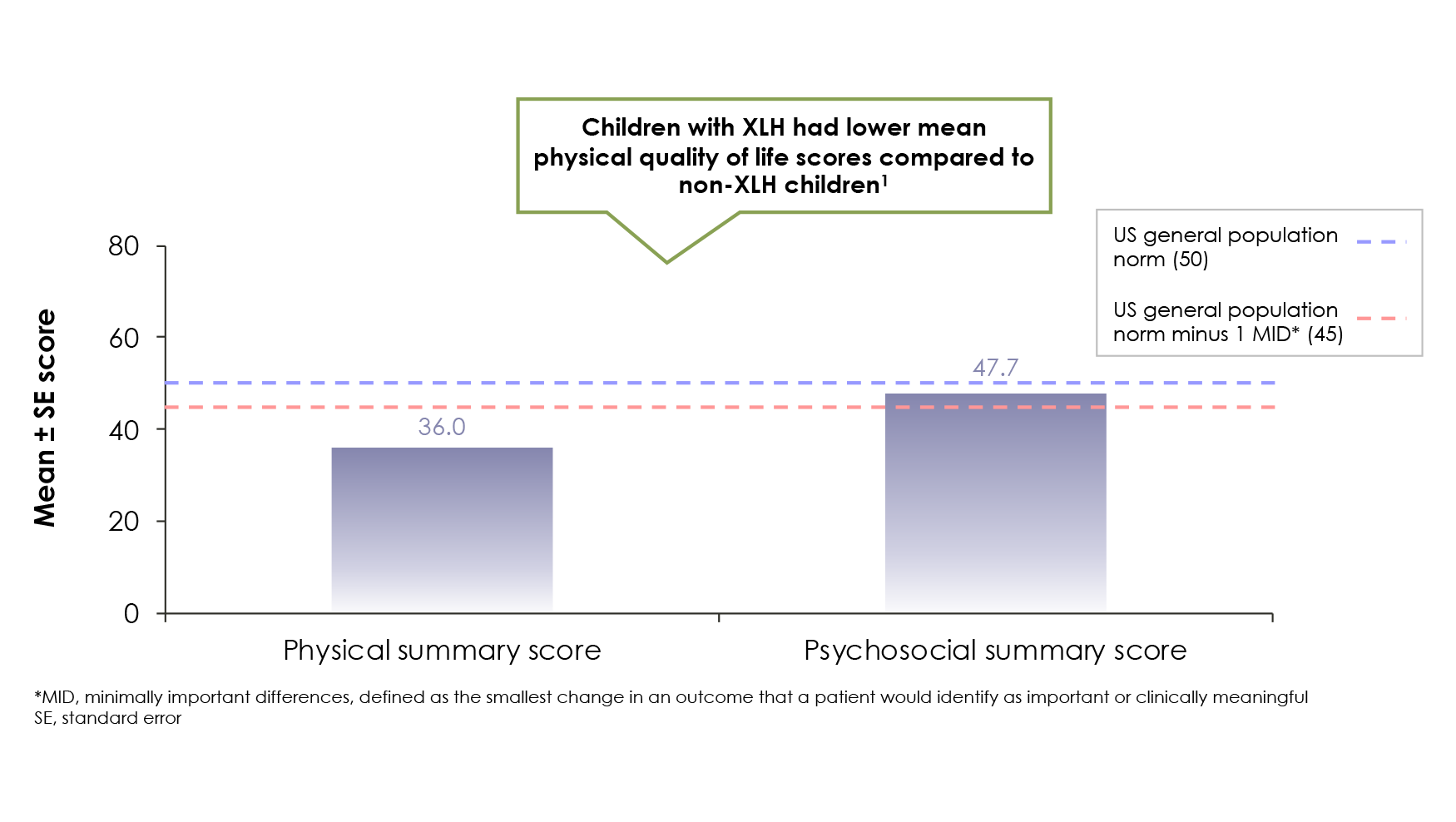
Data from the same survey showed children with XLH had heightened pain and impaired mobility relative to normal children1
1. Skrinar A, Dvorak-Ewell M, Evins A, et al. The lifelong impact of X-linked hypophosphataemia: results from a burden of disease survey. J Endocr Soc. 2019;3(7):1321-1334. 2. Pettifor JM. What's new in hypophosphataemic rickets? Eur J Pediatr. 2008;167(5):493-499. 3. Ruppe MD. X-linked hypophosphatemia. In: Pagon RA, Adam MP, Ardinger HH, et al, eds. Gene Reviews. https://www.ncbi.nlm.nih.gov/books/NBK83985/. Accessed October 20, 2017. 4. Linglart A, Biosse-Duplan M, Briot K, et al. Therapeutic management of hypophosphatemic rickets from infancy to adulthood. Endocr Connect. 2014;3(1):R13-R30. 5. Veilleux LN, Cheung M, Ben Amor M, Rauch F. Abnormalities in muscle density and muscle function in hypophosphatemic rickets. J Clin Endocrinol Metab. 2012;97(8):E1492-E1498. 6. Martin A, Quarles LD. Evidence for FGF23 involvement in a bone-kidney axis regulating bone mineralization and systemic phosphate and vitamin D homeostasis. Adv Exp Med Biol. 2012;728:65-83. 7. Che H, Roux C, Etcheto A, et al. Impaired quality of life in adults with X-linked hypophosphatemia and skeletal symptoms. Eur J Endocrinol. 2016;174(3):325-333. 8. Carpenter TO, Imel EA, Holm IA, Jan de Beur SM, Insogna KL. A clinician's guide to X-linked hypophosphatemia. J Bone Miner Res. 2011;26(7):1381-1388. 9. Econs MJ, Samsa GP, Monger M, Drezner MK, Feussner JR. X-linked hypophosphatemic rickets: a disease often unknown to affected patients. Bone Miner. 1994;24(1):17-24. 10. Zivičnjak M, Schnabel D, Billing H, et al. Age-related stature and linear body segments in children with X-linked hypophosphatemic rickets. Pediatr Nephrol. 2011;26(2):223-231. 11. Carpenter TO. New perspectives on the biology and treatment of X-linked hypophosphatemic rickets. Pediatr Clin North Am. 1997;44(2):443-466. 12. Opsahl Vital S, Gaucher C, Bardet C, et al. Tooth dentine defects reflect genetic disorders affecting bone mineralization. Bone. 2012;50(4):989-997. 13. Picture of the teeth: human anatomy. WebMD. https://www.webmd.com/oral-health/picture-of-the-teeth#1. Updated 2015. Accessed December 9, 2017.